Last week
it was announced that
Asante, makers of the Snap insulin pump, are the first diabetes device company to partner with
Tidepool, a non-profit working to reduce the burden of T1D, in an effort to make diabetes device data open and available to patients and their caregivers.
This is where I'm going to highly encourage you to check out
what Tidepool is doing, because it helps explain why this partnership with Asante is such a big, big deal.
I wanted to learn more about what exactly this partnership means, so I reached out to Asante and was able to chat with their CEO,
David Thrower, and then with the CEO of Tidepool,
Howard Look. They were kind enough to talk me through some of their vision for what this partnership could mean, and how it might improve the lives of PWDs.
What I learned is: yes,
this is HUGE.
Wait, nope, hang on. More emphasis required.
THIS IS HUGE.
For example: you know how if you wear one brand's pump but want to use another brand's CGM, you're stuck using two different proprietary software programs to upload and interpret your data - and maybe you can't even
access all of the data you want? Same goes for a glucose meter that works independently of your insulin pump or your CGM. They're all stand-alone devices, and most of them don't talk to each other. You're often forced to choose between using devices that the manufacturer has decided to integrate (a Medtronic pump and CGM, or an Animas Ping and their meter-remote, for example), or using the devices that you like best.
What if you were no longer bound by proprietary nonsense, and could choose devices based on what works best for you without being bound by what device-makers decide would work together? What if you could upload everything to one platform, and that platform could tell you everything about what your devices are capturing and recording - and help you decide what to do next?
What if that platform enabled you to use any number of apps, all of which were pulling data from
all of your devices?
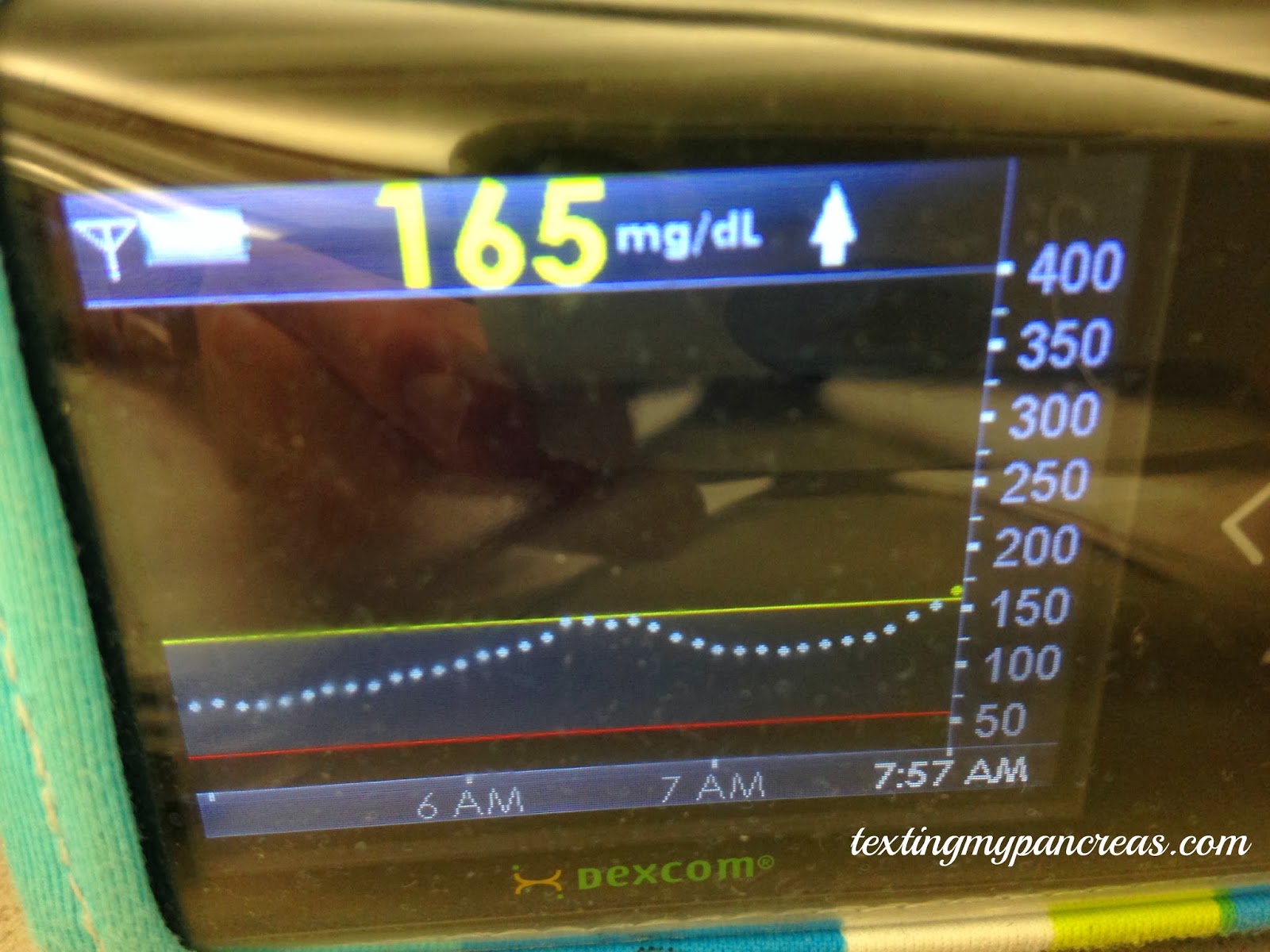
What if you could log into the cloud and see your child's CGM graph, in real time - while they're away from home?
 |
| A demo screenshot of what Tidepool's platform might let one see, moving in real time |
What if you could send that CGM graph to another device? What if the graph you could see belonged to your child; your spouse; your patient?
What if
your data was yours, and
you got to choose how to look at it and what to do with it?
 |
| A screenshot from Tidepool's first app, "blip". |
That's exactly what Tidepool is working to make a reality, and Asante has made a bold step in being the first device company to say, "yeah, we believe in this vision of open device data, too". As Tidepool's Look put it, "It's very apparent that there's a need for open data that PWDs and their caregivers can access in whatever way they want". Asante's Thrower echoed: "We founded Asante with the notion that diabetes comes with a constant and high cognitive load, and whatever we can do on our side to reduce that burden - to simplify the monitoring and treating of diabetes - that's what we ought to do".
And also from Thrower (I'm paraphrasing here): "In all of our strategies, let's treat people like people - not just consumers attached to a medical device. Their device choices should be based on what works best for them, not what works with what you already have. A logical extension of this is to make available to people whatever data is useful or that can inform their management decisions." And not in an endless, unintelligible spreadsheet, either - they want to present that data in a way that people can understand and use.
Can I get an amen!

So all of this sounds great, but isn't FDA going to need to approve this? (And the cynics in us lament,
and how long will that take?)
Yes, they will. And here's what they had to say: the key is engage early and often, and Tidepool has already met several times with FDA. Tidepool aims to classify their platform as a "
masterfile" with FDA, and any corresponding applications may or may not need subsequent FDA approval.
So what can we, as a community, do to help make sure this vision of open and accessible data becomes reality? Here is Tidepool's ask:
- If folks would like to stay in touch with updates, they can add themselves to our mailing list at tidepool.org and also follow us at @Tidepool_org and Facebook.com/TidepoolOrg .
- We are about to start a pilot study of blip at UCSF. If folks are patients at UCSF, they should talk to their doctors there.
- Open source developers should send us a note, info@tidepool.org. Soon we’ll have lots of ways they can contribute. They can also find our code repositories at GitHub.com/Tidepool-org, and our nascent developer portal at http://tidepool-org.github.io. We’d also love help from QA people, test developers, and documentation tech writers.
- Of course, as a non-profit, we warmly welcome donations to our efforts at tidepool.org/donate.
And here's where the business major in me raises its voice: I hope the market rewards companies like Asante for making bold steps like this. If this is truly the kind of revolution we want for ourselves,
we have to raises our voices.
(And remember - Asante is still offering those
four-week free trials with their insulin pump.)
Editor's Note: Neither Asante nor Tidepool solicited me to write about this. When I saw the news break last week I was surprised to not see more enthusiasm and excitement, so I'm assuming most people just didn't realize what had happened. This is my own effort to help spread the word.